| Cardiology, diagnostic imaging | |||
Combined MRI and echocardiography improves stroke diagnosis14 March 2007 Using both MRI and echocardiography to image the heart greatly improves the ability of physicians to identify the cause of stroke, especially cardioembolic strokes, the worst type. These strokes have a worse prognosis, producing larger, more disabling strokes that are more likely to recur compared to other types. The technique could revolutionise patient care.
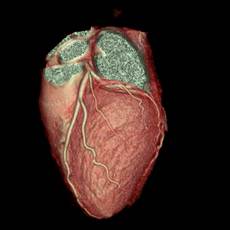
Based on a new study, researchers urge more comprehensive imaging for patients presenting to hospitals with stroke symptoms. Using both MRI and echocardiography to image the heart greatly enhances the detection of the cause and selection of the best treatment of cardioembolic strokes, the “meanest” type of stroke. A cardioembolic stroke occurs when a thrombus (clot) dislodges from the heart, travels through the cardiovascular system and lodges in the brain, first cutting off the blood supply and then often causing a hemorrhagic bleed — a double whammy of both types of stroke, ischemic first and then hemorrhagic. The study found that MRI detected nearly twice as many sources of stroke in the heart than echocardiogram alone. It also showed the ability of MRI to reveal more heart disease conditions that contribute to clot formation in the first place. Echocardiography, however, was strong in the detection of heart valve lesions. Combined, these imaging systems can more clearly identify underlying causes of future stroke, helping doctors decide the best initial therapy and the best treatment to prevent a secondary stroke. The research was presented today at the Society of Interventional Radiology’s 32nd Annual Scientific Meeting. "This can revolutionize patient care because we can detect the underlying cause of the stroke and prevent it from occurring again,” says lead author John Sheehan, M.D., an interventional radiologist at Northwestern University and Northwestern Memorial Hospital. “A potential cardiac source should be considered in all patients presenting with ischemic strokes. All stroke patients should routinely have an MRI and ultrasound of their heart, in addition to having their brain and carotids imaged with CT and MRI. It’s nice to be on the front end of a stroke – able to stop it, than on the back end, figuring out how to deal with its damage.” Stroke teams generally consist of emergency room physicians, neurologists, and interventional radiologists. Interventional radiologists are a critical part of the stroke team because they can diagnose and treat ischemic stroke with clot-busting drugs, or open a blocked carotid artery nonsurgically. They are also actively involved in creating more stroke teams across the country. Cardioembolic strokes, which account for 20 percent of embolic strokes, have a worse prognosis, producing larger, more disabling strokes that are more likely to recur compared to other types of stroke. Blood clots can be treated with drugs before they can leave the heart, in conjunction with treating identified heart conditions, to prevent another life-threatening stroke. In the United States stroke is the leading cause of adult disability and the third leading cause of death; only heart disease and cancer cause more deaths annually. In the study, of the 93 patients who had an MRI and echocardiogram of their heart after a stroke, MRI detected nearly twice as many potential causes of stroke originating from the heart compared to echocardiography. MRI also detected significant heart conditions that predispose a patient to stroke in 30 percent of patients compared to echocardiography. These additional findings included acute myocardial infarction, myocardial scarring, and left ventricular aneurysms. Echocardiography was, however, more sensitive to detecting potential embolic lesions on prosthetic cardiac valves and strokes related to a hole in the heart. (Abstract 132 can be found at http://www.SIRmeeting.org) “By using cardiac MRI and echocardiography to assess stroke patients, we have two sets of eyes: two ways to see what is causing the stroke to provide the best immediate care, and two ways to see what problems lie ahead for this patient that we could prevent with better long-term care,” Sheehan added. “The earlier we can detect underlying cardiac problems, the more quickly we can intervene to prevent future strokes. One stroke is more than enough. The chances of experiencing another stroke can be dramatically reduced by taking appropriate actions.” Definition of “stroke” and “cardioembolic stroke” A stroke occurs when the blood supply to a part of the brain is interrupted or severely reduced, depriving brain tissue of oxygen and nutrients. Within a few minutes, brain cells begin to die; as a result, abilities controlled by that area of the brain are lost. These abilities can include speech, movement, vision and memory. There are two basic types of stroke: ischemic (blockage of an artery) or hemorrhagic (rupture of an artery). About 80 percent of strokes are ischemic strokes. They occur when blood clots, plaque or vegetation block arteries to the brain and result in damage. Ischemic strokes are either embolic or thrombotic. Typically in an embolic stroke, a blood clot forms somewhere in the body, usually the heart, and travels through the blood stream to the brain. Once in the brain, the clot will continue traveling until it lodges in a small blood vessel blocking blood flow beyond that point, resulting in a stroke. This type of blood clot is called an embolus. A cardioembolic stroke occurs when the embolus has traveled from the heart. About 1 in 4 ischemic strokes are cardioembolic. The annual incidence of cardioembolic strokes in the U.S. is estimated at approximately 125,000 cases. These strokes can not be considered a single disease process as there are many different types of cardiac disorders that lead to cardioembolic stroke, each with unique clinical features, risks of initial and recurrent stroke, and optimal therapy. Causes of cardioembolic stroke A variety of heart diseases can predispose patients to the formation of clots within the heart, including atrial fibrillation, a recent heart attack, dilated cardiomyopathy (stretching and poor pumping action of the heart chambers), and diseases of the heart valves. These abnormalities can cause blood flow to slow down in parts of the heart; whenever blood slows, it tends to clot. In order to prevent these clots from forming, doctors put patients on medications that help reduce their occurrence. Specific cardiac risk factors include atrial fibrillation, acute myocardial infarction, left ventricular aneurysms, prosthetic heart valves and rheumatic heart disease. Atrial fibrillation (AF) is the most common heart condition that causes stroke. AF is caused when the two upper chambers of the heart (atria) beat rapidly and unpredictably. This causes the atrial walls to wriggle without contracting. Blood flow tends to slow down in this non-beating chamber, allowing clots to form. AF increases stroke risk up to six times. About 15 percent of all people who have a stroke have AF. Diagnosis of cardioembolic stroke Traditionally, an echocardiogram is used to evaluate the heart in stroke victims. Echocardiograms use ultrasound to look inside the heart for clots and other potential causes of cardioembolic stroke. Recently, magnetic resonance imaging (MRI) has emerged as a noninvasive imaging technique that can provide additional and complementary information to that obtained by echocardiography. MRI uses harmless magnetic fields that are used to take detailed pictures of the heart. It generates three-dimensional views of the heart, as well as surrounding organs, to create a larger diagnostic window into the patient’s health. The combination of MRI and echocardiography of the heart provides the optimal imaging assessment of stroke patients, leading to improved detection of not only the potential source of the stroke, but the underlying cause.
|